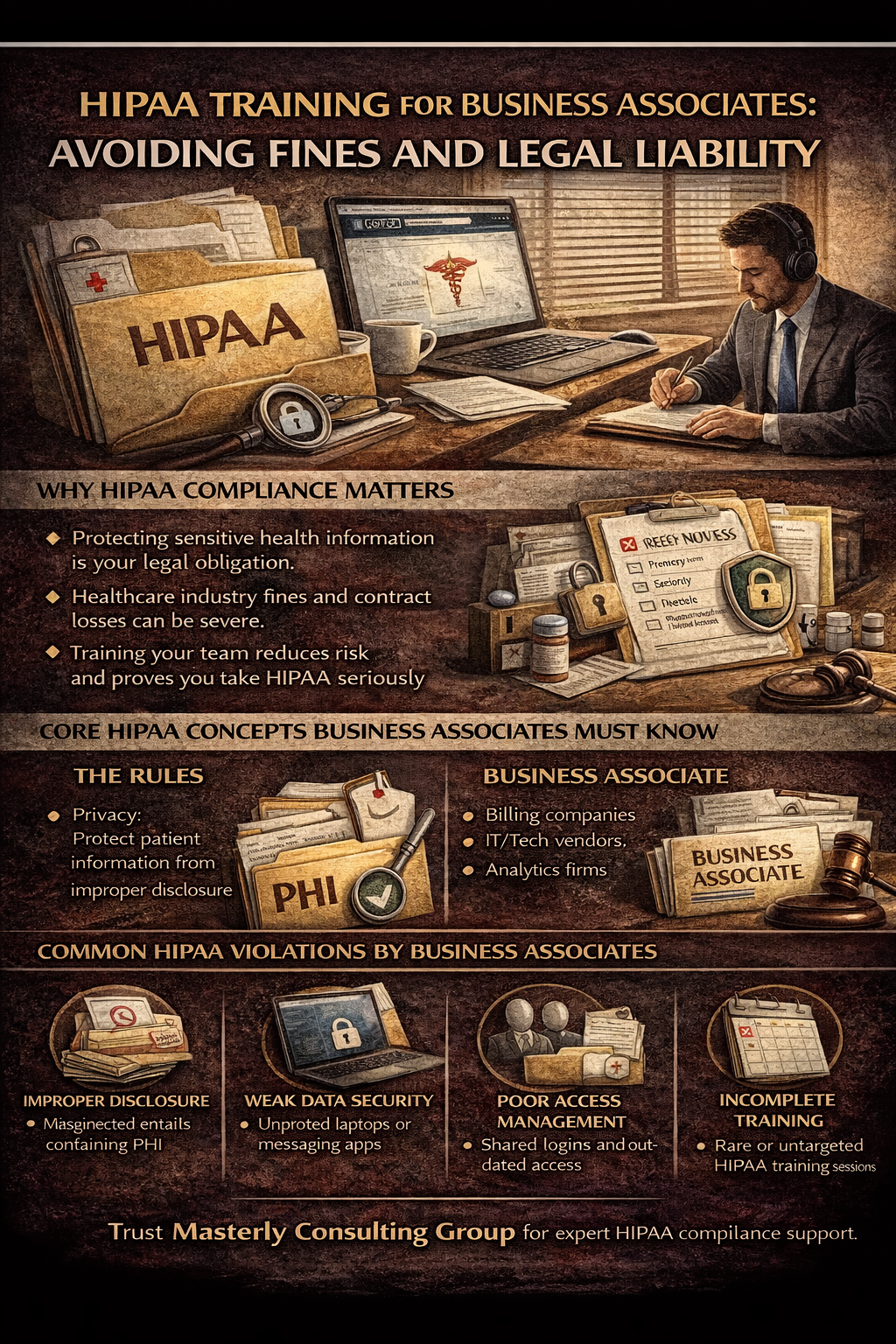
HIPAA Training for Business Associates: Avoiding Fines and Legal Liability
HIPAA risk rarely starts with a headline-making hack. More often, it starts with something ordinary: a rushed email, a shared login, a laptop left in a car, or a vendor who “only touches billing” assuming the rules don’t apply. In the healthcare industry, those small moments can turn into expensive problems fast—especially for businesses that support care delivery behind the scenes.
At Masterly Consulting Group, we help businesses build practical compliance programs that protect patient trust and reduce exposure. We work with teams that serve health care providers, health plans, and other healthcare organizations, and we’ve seen how quickly a well-meaning workflow can become a compliance gap. When business associates take HIPAA lightly, fines, contract termination, and reputational damage can follow.
This article explains what HIPAA expects from business associates, why training matters, and how to design privacy and security practices that actually work in the real world. The goal is not to scare you—it’s to help you protect your business, your clients, and the patient information you handle every day.
Why Business Associates Are Under More Scrutiny Than Ever
HIPAA enforcement has matured over the years, and regulators increasingly expect vendors to operate with the same seriousness as covered entities. A business associate isn’t “just a vendor” when they handle health information. They are part of a chain of trust that patients assume is secure.
When things go wrong, the question is rarely “Did you mean to?” The question is whether your compliance program was reasonable, documented, and consistently followed. Training is one of the first things investigators ask about because it shows whether your team understood their role.
Even if you outsource technology, you can’t outsource accountability. That’s why training has become a front-line risk tool for businesses in health care.
The Core HIPAA Framework in Plain Language
HIPAA is short for the Health Insurance Portability and Accountability Act, and it’s enforced through a set of rules and standards. Many compliance documents reference the insurance portability and accountability framework or the portability and accountability act as the foundation. The goal is to protect patient privacy, improve data security, and create clear responsibilities for organizations that handle medical information.
The Department of Health and Human Services oversees much of the enforcement structure. HIPAA connects with civil rights protections and other privacy laws because improper disclosure can cause real harm to patients.
If your business handles protected health information, HIPAA isn’t optional. It’s a legal requirement with real consequences.
What “Business Associate” Really Means
A business associate is typically a company that performs services for covered entities and uses or discloses protected health information to do that work. In practical terms, this can include billing support, IT support, analytics, transcription, legal support, and many operational services. You don’t need to be inside a clinic to be inside the compliance scope.
If you create, receive, maintain, or transmit patient data on behalf of a covered entity, you are likely acting as a business associate. That status triggers training, security standards, and documentation obligations.
The moment you touch medical records or related identifiers, you step into HIPAA territory. The rules apply whether you are large, small, remote, or onsite.
Covered Entities and Who You’re Serving
HIPAA uses the term covered entities to describe the organizations at the center of patient care and insurance operations. This includes many health care providers, health plans, and certain clearinghouse functions. Health insurance companies and healthcare providers often qualify, and they must ensure their vendors protect health information.
If your clients are covered entities, they will expect you to comply—and to prove it. That expectation usually appears in contracts, audits, and business associate agreements.
When covered entities are audited, their vendors often get pulled into the questions. Your compliance posture can affect your client relationships and renewal cycles.
Protected Health Information and Why It’s Bigger Than You Think
Protected health information isn’t just a diagnosis on a chart. It includes identifiers connected to a person’s health, care, or payment, and it can show up in more places than teams realize. A support ticket, a voicemail transcription, or a billing spreadsheet may contain patient data.
PHI exposure often happens in everyday tools—email, shared drives, project systems, and messaging apps. The more your team works fast, the easier it is to miss where protected data lives.
Training helps employees recognize PHI before they mishandle it. Recognition is the first step to privacy and security.
Health Information Privacy Is a Business Issue, Not Just a Legal One
Health information privacy affects contracts, partnerships, insurance, and reputation. A single incident can cause a client to pause work, require an expensive remediation plan, or terminate a relationship. Even if no fine is issued, the business damage can be significant.
Clients in health care want confidence that your procedures are consistent and your team is well-trained. They also want to see that you can respond quickly to security incidents without panic.
Privacy failures can lead to lost revenue and long-term trust issues. A training program is an investment in stability.
Why HIPAA Training Is the Fastest Risk Reduction Tool
Technology matters, but training is often the fastest path to fewer mistakes. Many data breach events start with user behavior—clicking a phishing link, sending an attachment to the wrong person, or using weak passwords. Good training reduces those everyday risks.
Training also supports regulatory compliance by proving your organization made reasonable efforts to comply. Investigators look for patterns: policies, training logs, and consistent enforcement.
A training program can also align your team’s decisions with your client’s expectations. That alignment protects relationships as much as it protects data.
HIPAA Training for Business Associates
hipaa training for business associates should be specific, role-based, and repeated often enough that it becomes normal—not a once-a-year slideshow. The training needs to reflect how your team actually works, what systems they use, and where they might encounter patient information. When training matches reality, compliance becomes easier.
It should also be documented, tested, and updated as workflows change. A policy that no one follows is not protection.
At Masterly Consulting Group, we help businesses build training that employees can apply on Monday morning. That’s how you avoid preventable HIPAA violations.
The HIPAA Rules Business Associates Must Know
HIPAA rules include expectations for limiting access, controlling disclosures, and maintaining security safeguards. They also set standards for how your organization responds when something goes wrong. The rules are not limited to hospitals—they apply across the business ecosystem that supports care.
Business associates must know what they can do, what they cannot do, and when they need permission. They also need to understand when something becomes an improper disclosure.
Training should translate HIPAA rules into daily decisions. That’s the difference between “knowing” and “complying.”
Privacy and Security: Two Sides of the Same Program
Privacy and security are often discussed separately, but in practice they’re connected. Privacy is about permitted use and disclosure, while security is about safeguards that protect systems and data. A privacy policy without security controls is fragile, and security controls without privacy awareness still leads to mistakes.
Business associates need both: rules about who can access patient information and systems that enforce those rules. Training bridges the gap by helping employees understand what the controls are for.
Strong privacy and security programs reduce confusion, especially during stressful situations. Clarity prevents accidental violations.
The Security Rules and What They Expect
HIPAA includes security rules that require administrative, physical, and technical safeguards. This doesn’t mean you need perfect systems, but it does mean you need reasonable protections for your size and risk profile. The standards focus on risk-based decisions and documented safeguards.
If you store health information in cloud tools, you need to understand access control, encryption, and monitoring. If you have remote employees, you need device and network standards.
Training should explain what safeguards exist and how to follow them. Security is a team sport.
Health Information Technology and the New Risk Surface
Modern health information technology is powerful, but it increases the attack surface. Integrations, APIs, shared tools, and remote workflows create more points of entry for attackers and more places where data can leak. Many businesses grow fast and add tools without updating procedures.
Training helps employees understand safe handling in the tools they actually use. It also teaches teams to recognize suspicious behavior and report it quickly.
With expanding health information technology, security issues can appear overnight. A prepared team is your best defense.
Business Associate Agreements Are More Than Paperwork
Business associate agreements define responsibilities, required safeguards, and breach response obligations. Many businesses sign them quickly without mapping the requirements into operations. That gap creates legal liability because contracts usually require specific behaviors, not vague intentions.
Your agreement may require employee training, audit cooperation, and defined reporting timelines. If you can’t meet those terms, you risk contract disputes and reputational damage.
Training should include what your agreement requires in plain language. It’s hard to comply with obligations your team doesn’t understand.
The Most Common HIPAA Violations Business Associates Trigger
HIPAA violations often come from predictable patterns. Teams are busy, tools are complex, and people make mistakes when they’re rushed. The most common issues include misdirected emails, poor access control, weak authentication, and unencrypted devices.
Other frequent HIPAA violations involve sharing logins, failing to terminate access for departed staff, and using personal devices without safeguards. These are preventable with training plus simple procedures.
When the same mistake repeats, regulators assume the program is weak. Training helps break those patterns before they become a finding.
Improper Disclosure Happens in Normal Workflows
An improper disclosure can be as simple as sending a patient file to the wrong email address or attaching the wrong document to a ticket. It can also happen when someone discusses patient details in a public area or uses unsecured messaging for convenience.
These issues aren’t usually malicious. They happen because people don’t recognize where the line is.
Training should include real examples from your workflow so employees can spot risk quickly. The goal is to prevent the “oops” moment.
Patient Privacy Is a Daily Practice
Patient privacy isn’t a poster on a wall—it’s how your team behaves under time pressure. When a support agent opens a ticket, when an analyst runs a report, or when a manager forwards an email, privacy decisions are being made.
The most effective programs treat privacy as a routine operational habit. That means clear procedures, clear access rules, and quick escalation paths when someone is unsure.
Your team should feel safe asking questions rather than guessing. Guessing creates HIPAA violations.
Privacy Practices That Keep Teams Consistent
Strong privacy practices create predictability. They define where data can be stored, how files are named, when encryption is required, and which tools are approved. They also define who can access which information and how long access is retained.
When practices are unclear, employees invent workarounds. Workarounds are where breaches and violations hide.
Training should reinforce these privacy practices regularly, especially as your tools and services expand.
Data Security and Why “Good Enough” Isn’t Good Enough
Data security in health care is not a vague goal; it’s a set of actions. You need controls that match your risk level, and you need proof those controls are active. This includes authentication, logging, endpoint protection, and secure configuration.
Many businesses assume their software vendor handles everything. But your organization is still responsible for access, user behavior, and internal controls.
Training should explain what your security controls are and why they matter. Employees protect what they understand.
Data Breach Reality: What Triggers Reporting Requirements
A data breach can involve unauthorized access, theft, loss, or improper exposure of protected data. Not every incident becomes a reportable breach, but you must evaluate quickly. The difference often depends on what data was involved, who accessed it, and whether it was actually acquired.
Your breach response plan should define how to assess risk and who makes the decision. Delays can create bigger liabilities and regulatory inquiries.
Training should teach employees how to report quickly and accurately. Speed is a major risk reducer.
Security Incidents and Why Response Time Matters
Security incidents include suspicious logins, malware alerts, lost devices, misdirected emails, and unauthorized access attempts. The faster your team reports them, the faster you can contain damage. Most major breaches become major because detection was slow.
Your incident response process should be simple enough that employees will actually use it. If reporting is confusing, people stay quiet.
Training should make reporting normal and non-punitive. You want fast reporting, not fear.
Incident Response and Breach Response Are Not the Same Thing
Incident response is the process of handling a suspected issue quickly. Breach response is what happens when the event meets the definition of a breach and requires formal actions. Many businesses mix these up, which leads to overreacting in some cases and underreacting in others.
A clean process helps teams stay calm and organized. It also provides documentation that supports regulatory compliance.
Training should clarify the difference and show employees what to do at each stage. Clear steps reduce chaos.
Regulatory Compliance Is Built on Documentation
Regulatory compliance isn’t just “doing the right thing.” It’s proving that you did it. Investigators and clients want documentation: training records, policies, access logs, and risk decisions.
Even strong controls can look weak if you can’t show evidence. Documentation also helps you improve over time because it reveals patterns.
Training should include the “why” behind documentation. People are more consistent when they understand the purpose.
Regulatory Inquiries and How They Usually Start
Regulatory inquiries often start after a complaint, a breach notification, or an audit trigger. Sometimes they begin because the HHS Office receives reports about patterns in an industry. Sometimes they come from a covered entity’s audit of its vendors.
The point is that inquiries can happen even if you believe your systems are fine. The question becomes whether you can show that you complied with HIPAA regulations.
Training, policies, and response plans become your story. You want that story to be strong and consistent.
The HHS Office and Why Business Associates Get Attention
The HHS Office that handles HIPAA enforcement is focused on patient protection and systemic improvement. When incidents occur, the office evaluates whether organizations made reasonable efforts to prevent them. If your team lacks training or controls, the office may view the failure as avoidable.
Even when fines aren’t issued, corrective action plans can be expensive. They can require new training, new controls, and ongoing reporting.
Being prepared reduces both cost and disruption. Preparation starts with training.
Health Plans, Health Insurance Companies, and Vendor Risk
Business associates often support health plans and health insurance companies through claims operations, member services, and analytics. These organizations handle massive volumes of health information, which makes vendor oversight strict. They may require proof of training, security standards, and incident response procedures.
If you want to win and keep contracts, your compliance posture matters. A strong program can become a competitive advantage in commercial transactions.
Training is part of your sales credibility. It shows you’re built for health care work.
Health Care Providers and the Practical Compliance Expectations
Many health care providers rely on vendors for technology, billing, scheduling, and operational support. These healthcare providers are responsible for their own HIPAA compliance and often pass requirements to vendors through contracts. If your procedures are weak, you can create risk for your clients.
That’s why providers often ask for security documentation and training proof. They want to know your team can handle patient information responsibly.
A strong compliance program protects both sides. It reduces friction and audit fatigue.
Patient Information and Medical Records Handling Basics
Patient information includes more than clinical notes. It can include appointment details, billing data, identification, and communications. When that data becomes part of medical records, the sensitivity increases and so do expectations.
Business associates should define where patient information can be stored, how long it can be retained, and who can access it. This should include a clear access policy and a process for removing access when roles change.
Training should cover these basics repeatedly. Repetition prevents the “I didn’t know” mistake.
Health Information Privacy and Security Training Must Be Role-Based
Information privacy and security training should reflect what each role actually does. A developer needs different guidance than a customer support rep. A manager needs different procedures than a contractor.
Role-based training reduces confusion and increases compliance. It also demonstrates thoughtful risk management if you face an audit.
A broad range of training modules can help your program scale. The goal is consistency without overloading employees.
State Privacy Laws and Other Privacy Requirements
HIPAA is federal, but state privacy laws and other privacy requirements can add complexity. Some state rules are stricter than HIPAA, and some impose separate reporting timelines. Businesses that operate across states must be careful not to assume one standard covers all.
This is where good legal resources and expert guidance matter. Your program should map the applicable law and procedures for your footprint.
Training should mention that HIPAA is not the only rule in the world. Awareness reduces accidental violations.
The HITECH Act and Why It Matters for Business Associates
The HITECH Act strengthened enforcement and expanded expectations around breach reporting and electronic health information. It also increased attention on security and accountability. Many modern HIPAA compliance programs treat HITECH as a key driver of enforcement posture.
If you handle health information technology systems, HITECH concepts often show up in risk discussions. It’s part of why regulators and clients focus so heavily on security.
Training should include the high-level impact of HITECH. It helps employees understand why the rules feel strict.
The Information Blocking Rule and Access Expectations
The information blocking rule is often discussed alongside health information access and interoperability expectations. While it’s not the same as HIPAA privacy, it intersects with how organizations handle health information and requests. Confusion in this area can create compliance and operational risks.
Your procedures should clarify when and how information can be shared, and when it cannot. That clarity supports compliance and protects patient trust.
Training should outline escalation paths for access questions. When unsure, employees should know where to go.
Privacy Laws, Civil Rights, and Patient Respect
HIPAA connects to broader values, including civil rights and dignity in care. Privacy isn’t just data—it’s respect for the patient. When privacy fails, patients can be harmed socially, financially, and emotionally.
That’s why privacy laws exist and why enforcement continues. Your team should see compliance as part of ethical service, not just a checklist.
Training that emphasizes patient respect tends to stick. People follow rules more consistently when they understand the human impact.
Risk Management: Where Training Fits
A strong compliance program is a risk management system. It identifies where things could go wrong, reduces likelihood, and reduces harm if something happens. Training is one of the most cost-effective controls because it targets the human layer.
Risk management also involves policies, technical controls, monitoring, and response. Training connects these parts into daily behavior.
When clients evaluate vendors, they evaluate maturity. Training is a visible maturity signal.
Security Standards That Are Realistic and Auditable
Security standards should be realistic for your team and measurable in practice. This includes password rules, MFA requirements, device encryption, and approved tool usage. If standards are too complex, people bypass them.
Auditors and clients prefer simple standards that are enforced consistently. Consistency prevents security issues and supports regulatory compliance.
Training should explain the standards and the reasons behind them. That improves adoption.
Access Control and “Least Privilege” in Practice
Access should be granted based on role and need. Too much access creates risk; too little access creates workarounds. Your program should define a clear access request and approval workflow.
This is especially important for contractors and temporary staff. A new contractor often receives broad access “just in case,” which can be dangerous.
Training should teach managers how to request access responsibly. Access control is one of the biggest compliance leverage points.
Security Issues That Start With Convenience
Many security issues start with convenience. Shared accounts, saved passwords, personal emails, and informal texting can feel easier than official tools. But convenience-based shortcuts are a common source of HIPAA violations.
Teams should have approved methods that are nearly as convenient as the risky alternatives. If your tools are painful, people will avoid them.
Training should address convenience head-on. It should offer safe shortcuts that still comply.
How to Build a Practical HIPAA Training Program
A training program should be short enough to complete, specific enough to matter, and frequent enough to be remembered. It should also include testing, documentation, and refreshers after policy changes.
A strong program usually includes:
- Onboarding training for new hires
- Annual refreshers and short quarterly reminders
- Role-based modules for different teams
- Phishing simulations and security awareness exercises
- Incident reporting drills and breach response walkthroughs
This approach keeps knowledge fresh without overwhelming staff. It also creates documentation that supports compliance.
Training New Hires Without Slowing the Business Down
Training should be part of onboarding, not an afterthought. A new employee needs to understand what PHI looks like, how to store it, and how to report issues. If they learn after an incident, it’s too late.
Onboarding should include practical examples tied to your tools. It should also include quick checks to confirm understanding.
This is one of the easiest ways to prevent early mistakes. New employees are high-risk simply because they don’t know your systems yet.
Working With Healthcare Organizations and Other Clients
Many businesses serve multiple clients with different expectations. Other clients may require different reporting timelines, different security documentation, or different tool approvals. Your training program should reflect those variations without becoming confusing.
The key is building a core program and layering client-specific rules when necessary. That protects consistency while respecting contracts.
When your team understands the big rules and the client-specific rules, mistakes decrease. That directly reduces legal liability.
When You Need a HIPAA Lawyer and When You Need Consulting Support
Sometimes businesses need counsel from a HIPAA lawyer—especially after a serious incident, regulatory inquiry, or contract dispute. Other times, businesses need operational help implementing compliance programs that work. The two roles are different but complementary.
Masterly Consulting Group focuses on helping businesses build functional compliance systems and training programs. We also understand when to involve legal counsel and how to coordinate with law firms when needed.
The right support depends on your situation and risk level. What matters is taking action before problems compound.
How Masterly Consulting Group Supports HIPAA Compliance
We support businesses across the health care ecosystem, including vendors serving health care providers and health plans. We bring extensive experience, deep knowledge, and a practical approach that respects how teams actually operate. We’ve advised clients on compliance design, training structure, and response planning in high-pressure environments.
Our work focuses on clear procedures, documentation, and repeatable workflows. We help clients protect patient data, reduce security risks, and respond confidently when issues occur. We also help align your program with HIPAA regulations, contracts, and reasonable security expectations.
When compliance becomes part of operations, it stops feeling like a fire drill. It becomes a stable business asset.
Contact Masterly Consulting Group for a Free Consultation
If your business supports the healthcare industry, handles protected health information, or signs business associate agreements, you need a compliance program that’s more than a policy binder. The fastest way to reduce risk is training that fits your real workflow, backed by procedures your team can follow under pressure. Whether you’re concerned about HIPAA violations, preparing for audits, or strengthening privacy and security safeguards, we can help you build a practical plan.
Contact Masterly Consulting Group at (888) 209-4055 to book a free consultation. We’ll discuss your current processes, where risk may be hiding, and how to create training and documentation that supports regulatory compliance and protects your client relationships.